
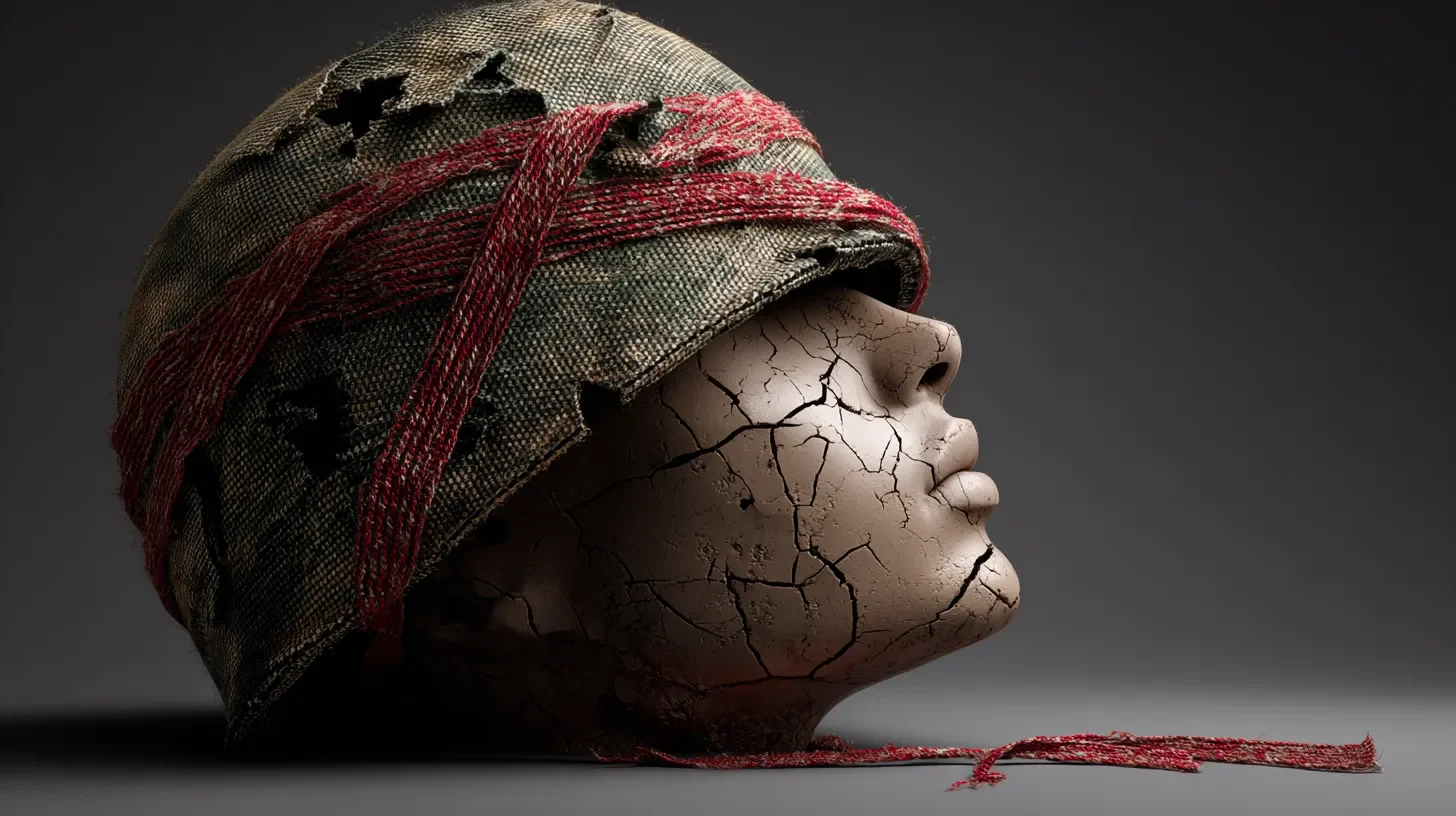
Post-Traumatic Stress Disorder (PTSD)
❝PTSD can develop after trauma, but with proper diagnosis and proven treatments, recovery and healing are possible.❞
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that develops after experiencing or witnessing a traumatic event. It causes lasting symptoms that disrupt daily life, relationships, and overall well-being. PTSD is a natural response to abnormal events and is treatable with proper care.
Therapy should be personal. Our therapists are qualified, independent, and free to answer to you – no scripts, algorithms, or company policies.
Find Your TherapistTable of Contents | Jump Ahead
What Is PTSD?
PTSD happens when your mind and body cannot recover properly from trauma. It is normal to feel upset or scared after trauma, but in PTSD, these feelings persist or worsen over time. The brain’s alarm system stays activated, making you feel unsafe even when you are not. Trauma changes how your brain handles memories and stress.
PTSD is not a sign of weakness or something you can simply "get over." It is a real medical condition affecting both body and mind. Many people with PTSD are strong survivors of difficult experiences.
What Causes PTSD?
PTSD can develop after events involving actual or threatened death, serious injury, or sexual violence. Not everyone exposed to trauma gets PTSD, but some risk factors increase the chance of developing it.
Types of Traumatic Events
- Combat exposure and military service
- Physical or sexual assault
- Serious accidents (car crashes, workplace accidents)
- Natural disasters (earthquakes, floods, hurricanes)
- Terrorist attacks or mass violence
- Childhood abuse or neglect
- Medical emergencies or life-threatening illnesses
- Sudden death of a loved one
- Being held captive or kidnapped
Risk Factors
Several factors can make you more likely to develop PTSD:- Previous trauma exposure - Having experienced trauma before
- Family history - Having relatives with PTSD or other mental health conditions
- Lack of support - Not having strong social support after trauma
- Additional stress - Dealing with other major stressors at the same time
- Mental health history - Having depression, anxiety, or other mental health conditions
- Substance use - Using alcohol or drugs to cope with stress
Protective Factors
Some things can help protect you from developing PTSD:- Strong social support from family and friends
- Healthy coping skills and stress management
- Seeking help early after trauma
- Having a sense of purpose and meaning
- Good physical health and self-care habits
Symptoms of PTSD
PTSD symptoms usually start within one month of a traumatic event, but they can appear months or even years later. To be diagnosed, symptoms must last more than one month and cause serious distress or interfere with daily life.
Re-experiencing Symptoms
These involve reliving the traumatic event:- Flashbacks - Feeling like the trauma is happening again, with vivid memories, sounds, or smells
- Nightmares - Disturbing dreams about the trauma or other frightening content
- Intrusive memories - Unwanted, distressing memories that pop into your mind
- Emotional distress - Intense upset when reminded of the trauma
- Physical reactions - Your body reacting (rapid heartbeat, sweating) to trauma reminders
Avoidance Symptoms
These involve staying away from trauma-related triggers:- Avoiding thoughts and feelings - Trying not to think or talk about the trauma
- Avoiding reminders - Staying away from places, people, or activities that remind you of the trauma
- Memory problems - Being unable to remember important parts of the traumatic event
- Emotional numbing - Feeling disconnected from your emotions or other people
Negative Changes in Thinking and Mood
These involve persistent negative thoughts and feelings:- Negative beliefs - Thinking badly about yourself, others, or the world ("I'm broken," "nowhere is safe")
- Distorted blame - Blaming yourself or others for the trauma or its consequences
- Persistent negative emotions - Ongoing fear, horror, anger, guilt, or shame
- Loss of interest - No longer enjoying activities you used to like
- Feeling detached - Feeling disconnected from family and friends
- Inability to feel positive emotions - Trouble experiencing happiness, satisfaction, or love
Changes in Physical and Emotional Reactions
These involve being overly alert or easily startled:- Hypervigilance - Being constantly on guard for danger
- Exaggerated startle response - Being easily frightened or startled
- Self-destructive behaviour - Drinking too much, using drugs, or taking dangerous risks
- Concentration problems - Trouble focusing or paying attention
- Sleep problems - Difficulty falling asleep, staying asleep, or restless sleep
- Irritability and anger - Verbal or physical aggression with little provocation
Types of PTSD
Acute PTSD
- Symptoms last between one and three months
- Often develops immediately after trauma
- May resolve on its own or with treatment
- Early intervention is important
Chronic PTSD
- Symptoms last longer than three months
- May continue for years without treatment
- Often requires professional help
- Can significantly impact daily functioning
Delayed-Expression PTSD
- Symptoms don't appear until at least six months after trauma
- May be triggered by additional stress or reminders
- Can occur years after the original trauma
- Sometimes called "delayed onset" PTSD
Complex PTSD (C-PTSD)
- Results from repeated, prolonged trauma
- Often involves childhood abuse or neglect
- Includes additional symptoms beyond regular PTSD
- May involve problems with emotional regulation and relationships
Diagnosis
PTSD is diagnosed by mental health professionals using specific criteria from the DSM-5-TR. The diagnosis requires:Diagnostic Criteria
- Exposure to trauma - Direct experience, witnessing, learning about trauma to a close person, or repeated exposure to trauma details
- Intrusion symptoms - At least one re-experiencing symptom
- Avoidance - Avoiding trauma-related thoughts, feelings, or reminders
- Negative mood and thinking changes - At least two symptoms of negative changes in thoughts and mood
- Arousal and reactivity changes - At least two symptoms of changes in physical and emotional reactions
- Duration - Symptoms lasting more than one month
- Functional impairment - Symptoms causing significant distress or problems in daily life
Assessment Process
When you see a mental health professional for a PTSD evaluation, they will:- Ask detailed questions about your trauma history
- Review your current symptoms and how long you've had them
- Assess how symptoms affect your daily life
- Rule out other mental health conditions
- May use standardised questionnaires like the PCL-5 (PTSD Checklist)
Treatment Options
PTSD is highly treatable, and most people can recover with proper care. Treatment often involves therapy, medication, or a combination of both.
Psychotherapy
Several types of therapy have strong evidence for treating PTSD:
Trauma-Focused Cognitive Behavioural Therapy (TF-CBT)
- Helps you process traumatic memories in a safe way
- Teaches coping skills for managing symptoms
- Challenges unhelpful thoughts about the trauma
- Usually involves 12-16 sessions
Eye Movement Desensitisation and Reprocessing (EMDR)
- Uses eye movements or other bilateral stimulation while recalling trauma
- Helps your brain process traumatic memories differently
- Often effective in fewer sessions than other therapies
- Doesn't require a detailed discussion of the trauma
Prolonged Exposure (PE) Therapy
- Gradually helps you face trauma-related memories and situations
- Reduces avoidance and fear responses
- Includes imaginal exposure (recounting trauma) and in vivo exposure (facing avoided situations)
- Usually involves 8-15 sessions
Cognitive Processing Therapy (CPT)
- Focuses on changing unhelpful thoughts about trauma
- Helps you understand how trauma affected your thinking
- Teaches skills for challenging negative thoughts
- Usually involves 12 sessions
Medications
Several medications can help reduce PTSD symptoms:
Antidepressants
- SSRIs - Sertraline (Zoloft) and paroxetine (Paxil) are FDA-approved for PTSD
- SNRIs - Venlafaxine (Effexor) may also be helpful
- Help with depression, anxiety, and sleep problems
- It may take 6-8 weeks to see the full effects
Other Medications
- Prazosin - May help reduce nightmares
- Anti-anxiety medications - For short-term relief of severe anxiety
- Sleep medications - To help with sleep problems
- Mood stabilisers - Sometimes used for irritability and anger
Other Treatments
- Group therapy - Connecting with others who have similar experiences
- Family therapy - Helping family members understand and support recovery
- Complementary approaches - Yoga, meditation, and acupuncture may be helpful alongside traditional treatment
Living with PTSD
Self-Care Strategies
- Maintain routines - Regular sleep, meals, and activities provide stability
- Exercise regularly - Physical activity can help reduce stress and improve mood
- Practice relaxation - Deep breathing, progressive muscle relaxation, or mindfulness
- Stay connected - Maintain relationships with supportive family and friends
- Limit alcohol and drugs - These can worsen PTSD symptoms
- Eat well - Good nutrition supports overall mental health
Managing Triggers
- Identify triggers - Learn what situations, people, or places trigger your symptoms
- Plan ahead - Have strategies ready for when you encounter triggers
- Use grounding techniques - Focus on your five senses to stay present
- Practice self-compassion - Be patient and kind with yourself during difficult times
Building Support
- Educate loved ones - Help family and friends understand PTSD
- Join support groups - Connect with others who understand your experience
- Consider peer support - Talk with others who have recovered from PTSD
- Maintain professional support - Regular check-ins with your treatment team
PTSD and Other Conditions
PTSD often occurs alongside other mental health conditions:
Common Co-occurring Conditions
- Depression - Persistent sadness and loss of interest
- Anxiety disorders - Generalised anxiety, panic disorder, or phobias
- Substance use disorders - Using alcohol or drugs to cope with symptoms
- Sleep disorders - Chronic insomnia or sleep disturbances
- Chronic pain - Physical pain that may be related to trauma
Treatment Considerations
- Treating co-occurring conditions often improves PTSD symptoms
- Integrated treatment approaches address multiple conditions simultaneously
- Medication choices may need to consider all conditions present
- Recovery may take longer when multiple conditions are present
Recovery and Prognosis
What to Expect
- Recovery is possible - Most people with PTSD can significantly improve with treatment
- Progress takes time - Healing from trauma is a gradual process
- Setbacks are normal - You may have good days and bad days during recovery
- Treatment works - Evidence-based therapies are highly effective for PTSD
Factors That Help Recovery
- Starting treatment early
- Having strong social support
- Using healthy coping strategies
- Staying engaged in treatment
- Taking care of your physical health
- Having hope and motivation for recovery
Long-term Outlook
With proper treatment, many people with PTSD:- Experience a significant reduction in symptoms
- Return to normal daily functioning
- Rebuild relationships and social connections
- Find meaning and purpose after trauma
- Develop resilience and post-traumatic growth
Prevention
After Trauma Exposure
While not everyone who experiences trauma develops PTSD, certain steps may help:- Seek support - Talk to family, friends, or professionals
- Take care of yourself - Maintain healthy habits and routines
- Avoid unhealthy coping - Don't use alcohol or drugs to cope
- Stay active - Engage in normal activities when possible
- Be patient - Allow yourself time to process and heal
Building Resilience
- Develop strong social connections
- Learn healthy stress management skills
- Practice self-care and maintain physical health
- Build a sense of purpose and meaning
- Develop problem-solving skills
When to Seek Help
You should consider getting help if you:- Have symptoms that last more than a month after trauma
- Feel like symptoms are getting worse instead of better
- Have trouble functioning at work, school, or in relationships
- Use alcohol or drugs to cope with symptoms
- Have thoughts of hurting yourself or others
- Feel like you can't handle your symptoms on your own
Getting Help
- Start with your primary care doctor
- Ask for a referral to a mental health professional
- Contact your local mental health centre
- Call a crisis hotline if you're in immediate distress
- Consider telehealth options if in-person care isn't available
Crisis Resources
- National Suicide Prevention Lifeline: 988
- Crisis Text Line: Text HOME to 741741
- PTSD National Centre: 1-802-296-6300
- Veterans Crisis Line: 1-800-273-8255
- Find a helpline, suicide hotline, or crisis line in your country: https://www.therapyroute.com/article/helplines-suicide-hotlines-and-crisis-lines-from-around-the-world
- Find an emergency ambulance number in your country: https://www.therapyroute.com/article/ambulance-emergency-numbers-worldwide-list-by-therapyroute
PTSD in Different Populations
Military Veterans
- Combat exposure is a common cause of PTSD in veterans
- Military culture may discourage help-seeking
- VA provides specialised PTSD treatment programs
- Transition to civilian life can be challenging
First Responders
- Police, firefighters, and paramedics have high rates of PTSD
- Repeated trauma exposure increases risk
- Peer support programs can be helpful
- Early intervention is important
Children and Adolescents
- PTSD can occur in children of any age
- Symptoms may look different from those in adults
- Play therapy and family involvement are important
- School-based interventions may be helpful
Survivors of Sexual Assault
- Sexual trauma often leads to PTSD
- Shame and self-blame are common
- Specialised trauma-informed care is important
- Support groups can be particularly helpful
Related Terms
- Trauma - The original disturbing experience
- Complex PTSD - PTSD from repeated trauma
- Acute Stress Disorder - Short-term reaction to trauma
- EMDR - A specific therapy for trauma
- Trauma-Focused CBT - Therapy approach for PTSD
References
American Psychiatric Association. (2024). What is Posttraumatic Stress Disorder (PTSD)?. https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd
American Psychological Association. (2024). Posttraumatic stress disorder. https://www.apa.org/topics/ptsd
American Psychiatric Association. (2013). Posttraumatic Stress Disorder - DSM-5. https://www.psychiatry.org/file%20library/psychiatrists/practice/dsm/apa_dsm-5-ptsd.pdf
StatPearls/NCBI. (2024). Posttraumatic Stress Disorder. https://www.ncbi.nlm.nih.gov/books/NBK559129/
This information is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of qualified health providers with questions about mental health concerns.
Important: TherapyRoute does not provide medical advice. All content is for informational purposes and cannot replace consulting a healthcare professional. If you face an emergency, please contact a local emergency service. For immediate emotional support, consider contacting a local helpline.
Creating Space for Growth: How Boundaries Strengthen Relationships
Setting boundaries in relationships is one of the most important yet often overlooked aspects of maintaining healthy connections with others. Boundaries are personal limi...
International Mutual Recognition Agreements for Mental Health Professionals
Table of Contents | Jump Ahead Executive Summary Part I: Bilateral Agreements Part II: Multilateral Frameworks Part III: Profession-Specific Frameworks Part IV: Assessmen...
Jumping to Conclusions
Table of Contents Definition Key Characteristics Theoretical Background Clinical Applications Treatment Approaches Research and Evidence Examples and Applications Conclus...
Case Conceptualisation
Table of Contents Definition Key Characteristics Theoretical Background Clinical Applications Conceptualisation Process International Perspectives Research and Evidence P...
Guided Discovery
Table of Contents Definition Key Characteristics Theoretical Background Clinical Applications Treatment Applications Research and Evidence Techniques and Methods Professi...
About The Author
TherapyRoute
Cape Town, South Africa
“Our in-house team, including world-class mental health professionals, publishes high-quality articles to raise awareness, guide your therapeutic journey, and help you find the right therapy and therapists. All articles are reviewed and written by or under the supervision of licensed mental health professionals.”
TherapyRoute is a mental health resource platform connecting individuals with qualified therapists. Our team curates valuable mental health information and provides resources to help you find the right professional support for your needs.

Related Articles

Prolonged Exposure
Prolonged Exposure therapy is one of the most rigorously researched treatments for PTSD, yet it is often misunderstood. Read on to learn how PE works, who it is best suit...

Healing PTSD Without Medication: How EMDR and CBT Help the Mind Recover
PTSD may follow trauma such as accidents or reserve duty, leading to nightmares, anxiety, and sleep problems. EMDR and CBT help the brain reprocess trauma and reduce dist...
Post-Traumatic Stress Disorder (PTSD): 2025 Statistics
PTSD affects millions around the world—but many don’t get the support they need to heal. This guide explores key global and U.S. statistics on who’s most affected, the ri...
